Retina and Vitreous
Pasadena Retina & Vitreous Treatment Options
Coastal Eye Associates provides a full spectrum of medical and surgical management of diseases affecting the back of the eye. Surgeons who specialize in this area have extensive experience in the treatment of retinal detachment, diabetic retinopathy, and macular degeneration. They are also highly skilled and experienced in the management of diseases and conditions such as retinitis pigmentosa, vascular occlusive disease, macular holes, hereditary retinal degenerations, ocular inflammation, penetrating trauma, and ocular tumors.

Diabetic Retinopathy
If you have been diagnosed with diabetes and are afraid of losing your vision, you are not alone. Diabetes has many faces—it affects people of all ages, races, and nationalities. Of the almost 20 million people in the United States with diabetes, almost half of those will eventually develop some sort of diabetic eye disease.
Diabetic retinopathy is the most common diabetic eye disease and a leading cause of blindness in American adults. It is caused by changes in the blood vessels of the retina.
If you have diabetic retinopathy, at first you may not notice changes to your vision. But over time, diabetic retinopathy can get worse and cause vision loss. Diabetic retinopathy usually affects both eyes.
What is Diabetic Eye Disease?
Diabetic eye disease refers to a group of eye problems that include diabetic retinopathy, cataract, and glaucoma, all of which are worsened by inadequate blood sugar control. Diabetic retinopathy is one of the leading causes of vision impairment among adults with diabetes. It is often without symptoms in its early stages, and vision changes may not occur until the disease has progressed severely.
Who is at risk for this disease?
All people with diabetes are at risk–those with Type I diabetes (juvenile-onset) and those with Type II diabetes (adult-onset).
During pregnancy, diabetic retinopathy may also be a problem for women with diabetes. It is recommended that all pregnant women with diabetes have dilated eye examinations each trimester to protect their vision.
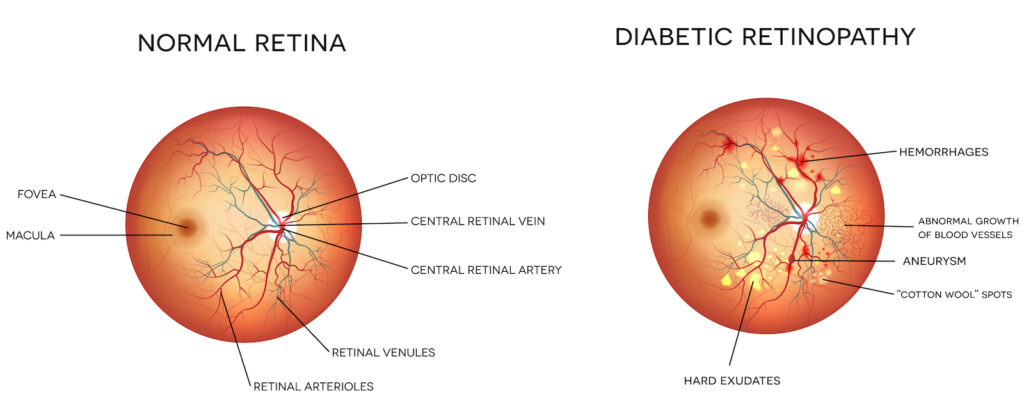
Diabetic retinopathy has four stages:
1. Mild Nonproliferative Retinopathy. At this earliest stage, microaneurysms occur. They are small areas of balloon-like swelling in the retina’s tiny blood vessels.
2. Moderate Nonproliferative Retinopathy. As the disease progresses, some blood vessels that nourish the retina are blocked.
3. Severe Nonproliferative Retinopathy. Many more blood vessels are blocked, depriving several areas of the retina with their blood supply. These areas of the retina send signals to the body to grow new blood vessels for nourishment.
4. Proliferative Retinopathy. At this advanced stage, the signals sent by the retina for nourishment trigger the growth of new blood vessels. This condition is called proliferative retinopathy. These new blood vessels are abnormal and fragile. They grow along the retina and along the surface of the clear, vitreous gel that fills the inside of the eye. By themselves, these blood vessels do not cause symptoms or vision loss. However, they have thin, fragile walls. If they leak blood, severe vision loss and even blindness can result
Symptoms
Often there are no symptoms in the early stages of the disease, nor is there any pain. Don’t wait for symptoms. Be sure to have a comprehensive dilated eye exam at least once a year.
Though vision may gradually become blurred, significant loss of sight does not usually occur with background retinopathy. Since the patient does not experience pain or external symptoms such as blood-shot eyes or discharge, changes in the retina can go unnoticed unless detected by an eye examination.
When bleeding occurs in proliferative retinopathy, the patient has a clouding or complete loss of sight. Connective tissue pulling on the retina causes distortion and blurring. However, if abnormalities occur in the peripheral retina, the patient may not experience any symptoms.

Normal Vision 
Diabetic Retinopathy
Treatment
Nonproliferative retinopathy does not require treatment. By controlling the levels of blood pressure, blood sugar, and cholesterol, the progression of nonproliferative retinopathy can be halted. However, if macular edema has begun, or if diabetic retinopathy has advanced to the proliferative stage, surgical treatment is usually required.
Laser Surgery
Laser Surgery is often helpful in treating diabetic retinopathy. To reduce macular edema, laser light is focused on the damaged retina to seal leaking retinal vessels. For abnormal blood vessel growth (neovascularization), the laser treatments are delivered over the peripheral retina. The small laser scars that result will reduce abnormal blood vessel growth and help bond the retina to the back of the eye, thus preventing retinal detachment. Laser surgery may be performed in your ophthalmologist’s office or in an out-patient clinic. Laser surgery can greatly reduce the chance of severe visual impairment.
Intraocular Steroid Injection
Intraocular Steroid Injection is a newly emerging treatment for diabetic macular edema. This therapy helps reduce the amount of fluid leaking into the retina, resulting in visual improvement. Due to the chronic nature of diabetic eye disease, this treatment may need to be repeated or combined with laser therapy to obtain a maximal or lasting effect.
Vitrectomy
When the growth of abnormal blood vessels in the retina has caused bleeding (vitreous hemorrhaging), a vitrectomy is usually required. This procedure removes blood clouding the vitreous gel at the center of the eye. During a vitrectomy, performed while the patient is under either general or local anesthesia, the ophthalmologist makes a very small incision in the eye, uses a tiny instrument to remove the vitreous gel, and replaces the gel with saline solution to restore clear vision. Typically done as an outpatient procedure, a vitrectomy requires the use of an eye patch and medicated eye drops for several days following surgery.
Retinal Detachment

What is Retinal Detachment?
The retina lines the inside of the eye like wallpaper. A retinal detachment occurs when the retina is pulled away from its normal position in the back of the eye. The retina sends visual images to the brain through the optic nerve. When detachment occurs, vision is blurred. A detached retina is a very serious problem that almost always causes blindness unless it is treated.
The retina normally lies smoothly and firmly against the inside back wall of the eyeball and functions much like the film in the back of a camera. Millions of light-sensitive retinal cells receive optical images, instantly “develop” them, and send them on to the brain to be seen. If any part of the retina is lifted or pulled from its normal position, it is considered detached and will cause some vision loss.
Who gets retinal detachment?
Retinal detachment develops in approximately 1 in 10,000 people per year. Certain conditions increase the likelihood of retinal detachment, including retinal breaks, posterior vitreous detachment, nearsightedness, eye injury, eye surgery, or a history of retinal detachment in family members. If a person has a retinal detachment in one eye, there is a 10% chance of eventually developing a detachment in their other eye.
What are the symptoms?
Symptoms of retinal detachment include painless:
- Floaters – Floaters are spots which patients perceive to be suspended or floating in their field of vision. Many patients describe these as a glob, a strand, a fly, pepper grains, or a web in their vision. They are best visualized against a white background and continue to float past the center vision after an eye movement
- Flashing lights – Flashes are like streaks of lightning which recur several times a day for several days. The flashes are a warning sign that something is happening to your retina. The vitreous (the gel like substance that fills your eye) can sometimes pull on the retina and cause an electrical signal to go to your brain. This signal lets you know that something different is happening in your eye.
- A curtain of visual loss that spreads across the field of vision. This may be transparent or opaque.
Vision loss can progress rapidly. Untreated, retinal detachment usually causes permanent blindness.
What is the cause?
Most retinal detachments develop after the gel (vitreous) in the cavity of the eye peels from the retina. Peeling of the vitreous gel (posterior vitreous detachment) is a normal age-related change that usually occurs after the age of 50. The vitreous gel can peel earlier in eyes that are very nearsighted, that recently underwent surgery, or have had a significant traumatic injury. A retinal tear can develop during the peeling of the gel due to an abnormal adhesion between the gel and the retina. A retinal tear allows fluid in the eye cavity to go through the tear to the space behind the retina where it can push the retina off the wall of the eye.
Breaks in the retinal tissue (retinal holes and retinal tears) are normally found in approximately 10% of people. In a small minority of persons with retinal breaks, liquid vitreous leaks beneath the retina, separating it from the eye-wall and causing a retinal detachment. A sudden separation of the vitreous from the retina (posterior vitreous detachment) is often the inciting event causing a retinal break or detachment. Macular pucker can also develop following a vitreous detachment.

How is it diagnosed?
Anyone who has sudden flashes, floaters, or peripheral vision loss needs an urgent examination by an eye doctor familiar with retinal diseases. A careful dilated retinal examination is necessary to diagnose retinal breaks or detachment.
A billowing retinal detachment surrounds the macula.
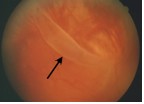
The retinal tear (arrow) causing this detachment is seen in the inferior retinal periphery.
How are retinal breaks and detachment treated?
Retinal breaks and tears
Retinal breaks and tears will usually need to be treated with laser surgery or cryotherapy (freezing), to seal the retina to the back wall of the eye again. These treatments cause little or no discomfort and may be performed in your ophthalmologist’s office. This treatment will usually prevent progression to a retinal detachment. Occasionally retinal tears are watched without treatment.
Retinal detachment.
Once the retina separates from the eye-wall it must be surgically pushed back into place; the causative retinal breaks are then “glued” with laser photocoagulation or cryotherapy. There are several surgical options available for repairing retinal detachment. Scleral buckling pushes the “wall against the wallpaper” whereas pneumatic retinopexy and vitrectomy push the “wallpaper against the wall.” Surgery is usually performed within a day or two of diagnosis, particularly if the macula and central vision are not yet affected.
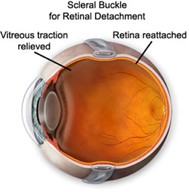
Scleral Buckle
A scleral buckle or flexible band is placed around the equator of the eye to counterbalance any force pulling the retina out of place. Often the ophthalmologist will drain the fluid from under the detached retina allowing the retina to return back to its normal position against the back wall of the eye. This procedure is performed in the operating room, usually on an outpatient basis.
Pneumatic retinopexy.
Pneumatic retinopexy describes the injection of a gas bubble into the vitreous space inside the eye enabling the gas bubble to push the retinal tear back against the wall of the eye and close the tear. Laser or cryo-surgery is used to secure the retina to the eye wall around the retinal tear. Your ophthalmologist will ask you to maintain a certain head position for several days. The gas bubble will gradually disappear. Sometimes this procedure can be done in the ophthalmologist’s office.
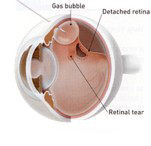
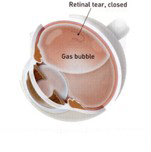
A gas bubble is injected into the vitreous with your head held steady in the right position, the gas bubble holds the retinal tear closed
Vitrectomy
Vitrectomy may be necessary to remove any vitreous gel which is pulling on the retina. This may also be necessary if the vitreous is to be replaced with a gas bubble. Your body’s own fluids will gradually replace this gas bubble, but the vitreous gel does not return. Sometimes a vitrectomy may be combined with a scleral buckle and or laser treatment.
What is the risk of surgery?
Retinal detachment is a sight threatening condition and surgery is necessary to repair the retina. Retinal detachment surgery is a complex procedure and may require different levels of treatment. Each person’s surgery may require more than one type of treatment. Your surgeon will review your options as well as the risks of surgery with you.
Will Your Vision Improve?
All retinal detachments are different. In general, if a retinal detachment can be fixed before the macula has detached, the visual prognosis is good. Several months may pass, however, before vision returns to its final level. The final outcome for vision depends on several factors. Therefore, close follow-up by your ophthalmologist is required. Patients usually need to have their glasses changed several months after retinal reattachment surgery.
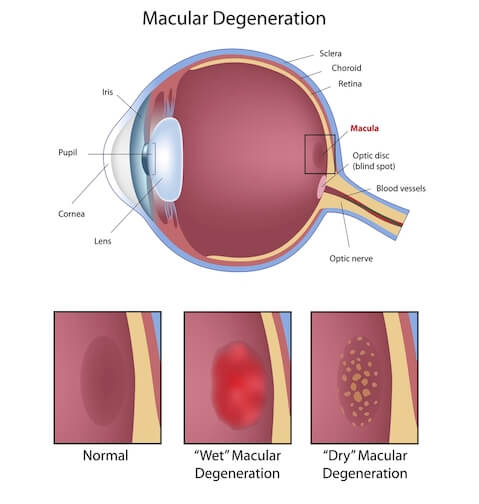
Macular Degeneration
Macular degeneration or age-related macular degeneration (AMD) is the leading cause of central vision loss in the Western world in persons over the age of 55. There are currently 15 million people in the United States with AMD and the incidence will increase to 25 million over the next 20 years as our population ages. AMD is, therefore, a growing public health issue.
Macular degeneration is caused by the deterioration of the central portion of the retina, the inside back layer of the eye that records the images we see and sends them via the optic nerve from the eye to the brain. The retina’s central portion, known as the macula, is responsible for focusing central vision in the eye, and it controls our ability to read, drive a car, recognize faces or colors, and see objects in fine detail.
There are two forms of macular degeneration
The Dry Type
This is the most common form. In this type of macular degeneration, the delicate tissues of the macula become thinned and cease to function properly.
The Wet Type
This is less common but is typically more damaging. The wet type of macular degeneration is caused by the growth of abnormal blood vessels behind the macula. The abnormal blood vessels tend to hemorrhage or leak, with the result being the formation of scar tissue if left untreated. In some instances, the dry type of macular degeneration can turn into the wet type.
Dry Macular Degeneration (non-neovascular).

Dry AMD is an early stage of the disease and may result from the aging and thinning of macular tissues, depositing of pigment in the macula, or a combination of the two processes.
Dry macular degeneration is diagnosed when yellowish spots known as drusen begin to accumulate from deposits or debris from deteriorating tissue primarily in the area of the macula. Gradual central vision loss may occur with dry macular degeneration but is not nearly as severe as symptoms associated with the wet form of AMD.
No FDA-approved treatments are available for the dry form of macular degeneration. A large, well-designed study (age-related eye disease) has concluded that high levels of dietary supplements consisting of a combination of vitamin C, vitamin E, beta carotene and zinc at specific concentrations may lower the risk of developing advanced stages of macular degeneration by 25% for people at high risk.
Wet Macular Degeneration (neovascular).

Leaking blood vessels cause fluids build-up, detaching cone and pigment cells. Vision loss can be sudden.
In about 10 percent of cases, dry AMD progresses to a more advanced and damaging form of the eye disease known as wet macular degeneration. With wet AMD, new blood vessels grow (neovascularization) beneath the retina and leak blood and fluid. This leakage causes permanent damage to light-sensitive retinal cells, which die off and create blind spots in central vision.
Neovascularization, the underlying process causing wet AMD and abnormal blood vessel growth, is the body’s misguided way of attempting to create a new network of blood vessels to supply more nutrients and oxygen to the eye’s retina. But the process instead creates scarring, leading to sometimes severe central vision loss.
Wet forms of macular degeneration are further classified into two general types:
- Classic: When blood vessel growth and scarring has very clear, delineated outlines observed beneath the retina, this type of wet AMD is known as classic choroidal neovascularization (CNV) usually associated with more severe vision loss.
- Occult: New blood vessel growth beneath the retina is not as pronounced and leakage is less evident in the occult CNV form of wet macular degeneration, which typically produces less severe vision loss.
Symptoms and Signs
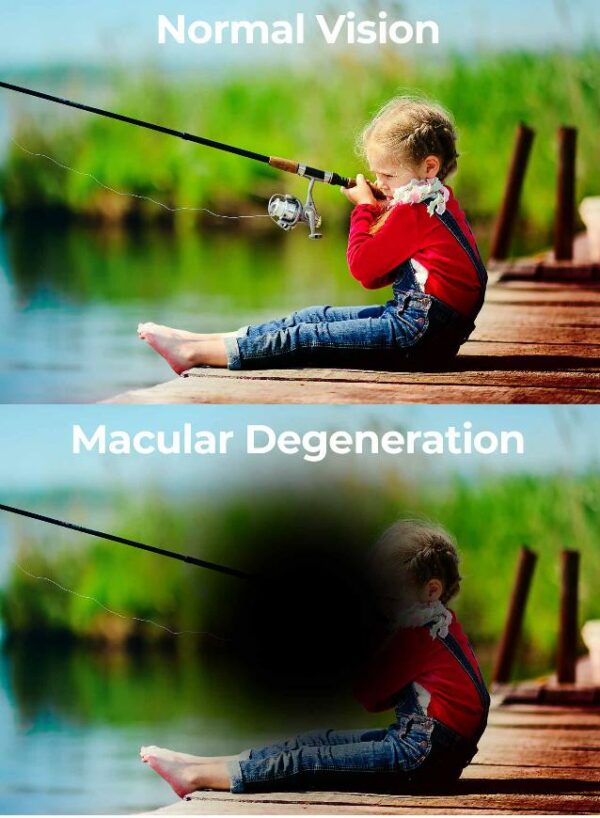
Macular degeneration develops differently in each person. Because it will affect different regions of the macula from person to person, the symptoms tend to vary. Macular degeneration causes a progressive loss of central sight, however, it does not cause total blindness. Peripheral vision is unaffected allowing a certain amount of mobility in normal surroundings. If left untreated, the wet type of macular degeneration may progress rapidly.
Symptoms often associated with macular degeneration include:
- A gradual loss of ability to see objects clearly
- A gradual loss of clear correct colors
- Vision that is noticeably distorted
- Straight lines appear wavy
- A dark or empty area appearing in the center of vision
- Difficulty reading or seeing objects up close
- Objects may appear the wrong shape or size
The symptoms described above may not necessarily mean that you have macular degeneration. However, if you experience one or more of these symptoms, contact your eye doctor for a complete exam
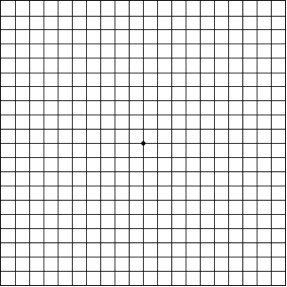
Viewing a chart of black lines arranged in a graph pattern (Amsler grid) is one way to tell if you are having these vision problems.
Testing Your Vision with the Amsler Grid
You can check your vision daily by using an Amsler grid like the one pictured below. You may find changes in your vision that you wouldn’t notice otherwise. Putting the grid on the front of your refrigerator is a good way to remember to look at it each day.
To use the grid: (click here for a printable copy)
1. Wear your reading glasses and hold this grid at 12-15 inches in good light.
2. Cover one eye.
3. Look directly at the center dot with the uncovered eye.
4. While looking directly at the center dot, note whether all lines of the grid are straight or if any areas are distorted, blurred or dark.
5. Repeat this procedure with the other eye.
6. If any area of the grid looks wavy, blurred or dark, contact the Coastal Eye physicians immediately.
Treatments for Macular Degeneration

Careful monitoring of vision and regular eye exams are important for those with both forms of ARMD. Dietary modifications are also important to help prevent the dry form of the disease from worsening.
A new class of drugs, known as anti-VEGF medications, has been shown to slow and even reverse the progression of the disease in some patients. This form of therapy is designed to inhibit the unwanted blood vessel growth caused by ARMD, thereby reducing leakage and bleeding. Examples of new therapies that we now offer include Avastin®, Lucentis®, and Macugen®.
Another treatment for wet ARMD is Photodynamic Therapy (PDT), a laser treatment that uses a light-activated drug called Visudyne. The drug is injected into an arm vein and travels through the bloodstream to the retina, where it is activated by a non-thermal laser. A clot is formed, closing the leaking blood vessels with minimal scarring to the retina.
Previous laser treatments for wet ARMD were successful in preventing loss of vision but caused scarring and damage to the retinal tissue. PDT allows the laser beam to focus on the area where the drug has concentrated and very quickly treat it, eliminating the likelihood of damage. The treatment may be reapplied if necessary.